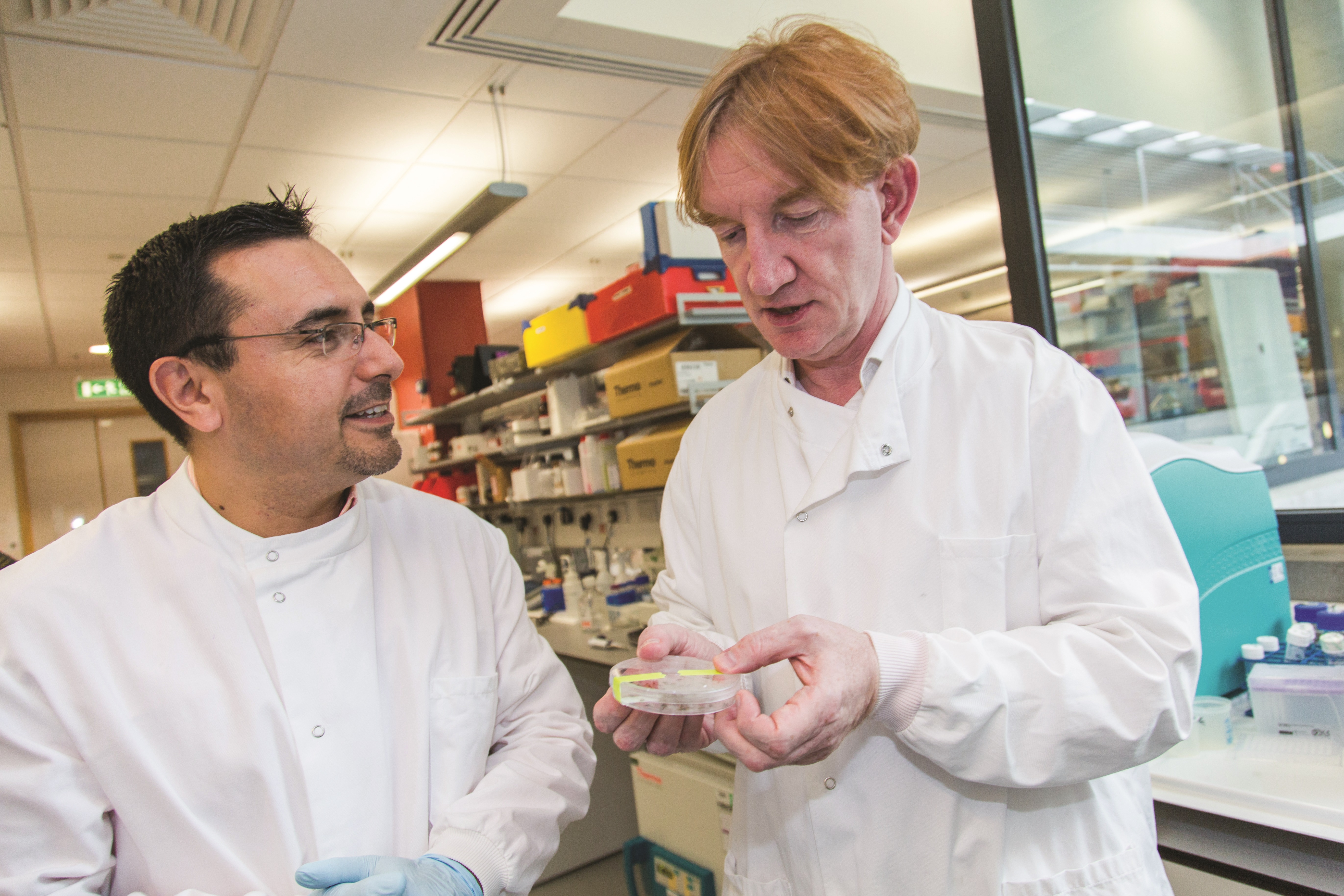
Adrian Hill [right] discusses an experiment with a colleague in the lab. They are focusing on improving vaccines for malaria, HIV and tuberculosis.
ENHANCING THE IMMUNOGENICITY AND EFFICACY OF VECTORED VACCINES
- Jan 1, 2016
- Download Retrospective

A post-doc in the Hill lab conducts a mosquito dissection using a microscope.
Adrian Hill, University of Oxford, United Kingdom
Adrian Hill's career as a scientist is defined by a single-minded passion: to develop a vaccine against malaria. It has driven him ever since he was a young geneticist in the late 1980s when he traveled several times to a hospital in The Gambia to study the disease.
"There were few doctors, and at times no antimalarial drugs," says Hill, director of the Jenner Institute at the University of Oxford. "You could only watch as children died." A vaccine to protect against the malaria parasite, Plasmodium falciparum, ranks as one of the most important goals in global public health. The mosquito-borne infection kills more than 600,000 children a year in Africa. And 25 years after he came face to face with the human tragedy caused by the parasite, Hill and his colleagues have created one of the most promising vaccine candidates.
In preliminary clinical trials with healthy volunteers, Hill's experimental vaccine has prevented the onset of malaria infection and disease in 20 percent of test subjects.[1] A subsequent larger trial in 121 men in Kenya found that the vaccine reduced the risk of infection by 67 percent.[2] As impressive, it also results in the elimination by the immune system of more than 90 percent of liver cells infected by the malaria parasite[1]. By eliminating cells already infected, the vaccine reduces the amount of parasites that can exit the liver and cause life-threatening complications.[3]
The response in liver cells is important because once the malaria parasite enters the bloodstream after a mosquito bite it races to the liver. There it infects the liver cells and uses them as a factory to produce swarms of the pathogen, which swamp the bloodstream, killing red blood cells and causing severe anemia. Under these conditions, children often die.
The vaccine's progress has been supported in a large part over the past decade by a $10 million grant from the Bill & Melinda Gates Foundation's Grand Challenges in Global Health program, building on about $20 million of support from the Wellcome Trust, the UK Medical Research Council and the European Commission. The vaccine is the first of its kind to induce the human immune system to produce a potent cellular immunity attack by CDS T cells that are capable of identifying liver cells infected by the parasite and destroying them before they can unleash an army of pathogens into the bloodstream.
"We've been good at firing up one arm of the immune system that produces antibodies," Hill says. "But what we realized as far back as the early 1990s is that we may need the other arm, cellular immunity, to protect against viruses like HIV, as well as tuberculosis and malaria." Antibodies are proteins that patrol the bloodstream and lock onto microbe particles and sweep them up. Since antibodies alone may not be able to wipe out an entire population of parasites that infest the blood derived from the bite of an infected mosquito, any amount of the microbe that reaches the liver can be enough to cause disease. To prevent disease, therefore, the body may require a second, back-up response from cellular immunity-generated T cells.
"Producing potent cellular immunity by immunization has been a 20-year obsession for me," Hill says."
Hill hit on a strategy by the late 1990s to induce cellular immunity to target an infected liver by administering, via injection into human volunteers, the DNA of a protein fragment of the parasite. The idea was that the DNA contained in a saline solution would stir the body's cellular machinery to convert the genetic material into the protein fragment-called an antigen-that would trick the immune system into reacting as if a pathogen invasion was underway. In a two-shot approach Hill developed by 2000, volunteers were first given the DNA injection to kick-start an immune system reaction. This "prime" inoculation was followed by a second booster shot of the same DNA inserted into modified vaccinia virus Ankara (MVA). Following years of experiments, Hill had found that using the MVA strain as a vector containing the antigen's DNA spurred an additional potent cellular immune response.[4] By this time, Hill had tested numerous parasite proteins to determine which fragment of the pathogen was best at eliciting just the right T cells. As important, he also made use of a fast and safe way to test in a small number of healthy volunteers whether each new version improved the cellular response. The volunteers were recruited at the Jenner Institute campus in Oxford, where they first were administered the two-shot "prime-boost" vaccine, and then were exposed to five bites from mosquitoes carrying the malaria parasite. Hill and his colleagues analyzed the subjects' blood to determine if each new iteration of the vaccine spurred greater amounts of T cells than the previous versions had. As the T cells alone were never fully protective, infected volunteers were then treated with antimalarial drugs so they didn't become sick.
In this way, after comparing many antigens both in the lab and in field studies of people naturally exposed to malaria in Africa, by 2001 Hill and his laboratory found that the best available T cell-inducing antigen was one called TRAP, a molecule from the parasite that appeared in liver cells after they were infected. Liver cells naturally expose TRAP to the immune system to trigger a protective T-cell attack, but the amounts of T cells generated naturally by humans this way are rarely enough to prevent disease. By delivering the fragment first via the DNA in saline and then via the DNA contained inside the MVA vector, Hill hoped to stimulate a large enough number of T cells to be protective.
In 2003, the first field trial of the "prime-boost" vaccine in almost 300 volunteers in The Gambia prompted a T-cell response. But after 11 weeks, the vaccinated adults weren't any less likely to develop malaria than a control group that had not been vaccinated.[5] "The good news is we got a T-cell response in nearly everyone," Hill says. "The bad news was - it wasn't enough."
At this time, Hill sought the Grand Challenges in Global Health grant to bolster his laboratory with graduate and post-graduate researchers to search for additional components, called adjuvants, that if added to the vaccine would significantly increase the numbers of T cells induced by the vaccine. "The Grand Challenges in Global Health grant allowed us to take a step back and ask what's really needed to make a major step forward in making a powerful, potent cellular immune response, going back to the drawing board if you like and trying a whole variety of new approaches," Hill says. "There was a huge risk this would yield absolutely nothing."
Using funds from the Grand Challenges in Global Health five-year grant, Hill's laboratory mined the human genome, eventually identifying more than 70 different adjuvant candidates, and testing even more combinations of adjuvants and antigens.
The laborious and tedious task of testing version after version finally paid off.[6] "In the end we found two approaches that produce a very potent cellular immune response," Hill says. "Before we started, we had no idea which two that would be."
The Hill research group then added the best of the adjuvants they had uncovered during the years of laboratory experiments to their TRAP malaria vaccine and moved forward to clinical testing of the adjuvants.
While the Grand Challenges in Global Health grant supported this laboratory research, the clinical tests in volunteers at the Jenner Institute and in field trials that assessed T-cell production of a sequence of new vaccine approaches were supported with grants from the UK Medical Research Council, the European Commission, the European Vaccine Initiative and the Wellcome Trust.
But two years into the five-year grant, "Adrian hadn't made the progress we had hoped," says Stephanie James, the grant's project manager at the Foundation for the National Institutes of Health. Hill was eliciting T cells, but not enough to be protective. "There was a lot of searching, searching, searching."
Hill himself realized he needed to find better vaccine vectors to contain the TRAP antigen and stimulate a more potent immune response than the DNA alone. Since viruses can naturally induce a strong immune response on their own, a weakened virus carting the antigen into the body very efficiently would likely improve T-cell production, he reasoned. Collaborating with scientists from the University of Pennsylvania he had found that particular viruses from chimpanzees showed real promise as vectors but these were not available for clinical development. The answer finally came in 2006, after Riccardo Cortese, chief executive and founder of Okairos AG, a Swiss-based biotech company, traveled to the Jenner Institute to present evidence that his company had independently developed a similar virus vector that might work.
Merck, the U.S. pharmaceutical company, previously had used a weakened adenovirus, a virus that causes respiratory and gastrointestinal ills in people, as a vector to elicit potent T cells in an experimental AIDS vaccine. The adenovirus was employed because it naturally triggers T cells, and because researchers had figured out relatively simple ways to insert antigen genes into it. Hill was reluctant to use human adenoviruses as vaccine carriers in Africa because people there were frequently exposed to these, so their protection would be blunted.
"Adrian's contribution has been to show in clinical trials that inducing T cells against the parasite can be very powerful," says Ashley Birkett, director of the PATH Malaria Vaccine Initiative.
However, Okairos, under Cortese's direction, had a different solution: a similar adenovirus that infected chimpanzees. Cortese had developed the approach at a laboratory in Rome owned by Merck. When Merck decided not to pursue chimpanzee virus research, Cortese created Okairos to develop the antigen-carrying platform himself. Between 2007 and 2010, Hill and Okairos working together produced a new version of the prime-boost vaccine that contained TRAP inside the chimp adenovirus, plus the MVA vector also containing TRAP.
While the DNA vaccine regimen had induced cellular immunity of about 400 T cells per milliliter of blood, the new "chimp-adeno" version generated more than 2,000 T cells per milliliter[1] Both components were needed: the "chimp-adeno" vector to start off the immune response and the MVA, which increased it five-fold. Hill says that eventually he wants to create a vaccine that elicits 10,000 T cells per milliliter. "I believe that's what's needed to block any of the parasites from leaving the liver." By the end of 2014, using grants from the Wellcome Trust and the British government, the Hill team had conducted several tests of the new chimp-adeno prime-boost vaccine in adults and young children, showing the vaccine to be safe and to generate an immune response.[7]
A scientist works at the 'dry box' during a research project at the Jenner Institute, University of Oxford.
In addition to showing that the vaccine reduced the risk of infection by 67 percent in the study involving 121 Kenyan men,[2] Hill's team estimated that the vaccine killed more than 90 percent of infected liver cells.[1]
"Adrian's contribution has been to show in clinical trials that inducing T cells against the parasite can be very powerful," says Ashley Birkett, director of the PATH Malaria Vaccine Initiative, which promotes research in the field. "As of now, it's one of the two most advanced approaches we have."
In June 2013, the British pharmaceutical company, GlaxoSmithKline (GSK) Pie, bought Okairos in a $325 million deal little noticed in the financial press. In the world of vaccine research, the acquisition was big news because it validated Hill's prime-boost regimen as a way to spur T cells. GSK says it plans to use the chimp-adeno technology as the foundation for vaccines against cancer, tuberculosis, hepatitis C, HIV and also malaria. The Jenner Institute is also progressing its own HIV and TB vaccines employing a different chimp-adeno vector developed in-house.
In a separate yet related development, Hill has recently begun testing in healthy volunteers a combination of the chimp-adeno vaccine with GSK's most recent version of its long-studied antibody-producing RTS,S vaccine. In several large trials in Africa, RTS,S has reduced the incidence of a malaria infection by as much as 30 to 50 percent.[8] "It's conceivable the two vaccines together might protect as many as 70 percent of recipients," says Ripley Ballou, a GSK official involved in the RTS,S project.
Finally, in an unexpected bonus, Hill's team has helped create a version of the vaccine that might not need to be refrigerated, often a challenge in getting vaccines to distant locales in poor countries where resources are limited. "The technology is based on a mixture of vaccine with simple sugars that is then dried on a thin paper membrane. That makes the vaccines thermostable, so they are able to stay potent at 37 degrees centigrade, human body temperature, for 12 months," Hill says. "That's unprecedented".[9]
Hill is optimistic that the combination of the chimp-adeno with MVA and RTS,S vaccines has the best chance yet of being the first "high-efficacy deployable malaria vaccine," he says. "If we do get to the finish line, the Grand Challenges in Global Health program will have been a significant contributor."
THE SCIENCE:
Inducing protective CD8+ T cell-immunity to malaria by a heterologous prime-boost vaccination approach
Adrian Hill and colleagues are harnessing cellular immunity to boost malaria vaccine efficacy. They analyzed different approaches to induce potent antigen-specific CD8+ T cells targeting liver-stage malaria parasites, which are thought to be particularly vulnerable to immune attack. CD8+ T cells producing interferon gamma IIFN-y) identify and kill host cells infected with pathogens such as Plasmodium. CD8+ T-cell responses can be induced by delivering liver-specific malaria antigens such as thrombospondin-related adhesion protein (TRAP) from P. falciparum with replicating and non-replicating viral vectors including human adenoviruses and the poxvirus, modified vaccinia virus Ankara (MVA). However, protection may be short-lived, and in many people, pre-existing neutralizing antibodies against the commonly used human adenovirus serotypes impair the T-cell response.
To enhance protection they developed a heterologous prime-boost regimen involving sequential administration of an adenovirus from chimpanzees (ChAd), which was shown to elicit a safe and potent protective immune response in humans,[10] followed by MVA, both carrying the modified malaria antigen, ME-TRAP[4] (TRAP fused to 20 mainly CD8+ T-cell epitopes from pre-erythrocytic antigens). With this approach they could induce better immune responses and longer-term sterile protection against malaria in mice,[11] rhesus macaques,[12] and humans.[1], [13], [14] In the human Phase Ila trial, their prime-boost approach using the chimpanzee adenovirus provided a significant protection rate against malaria (3 out of 14 vaccinees were sterilely protected, one of whom remained protected for 8 months), which was higher than in all other comparable trials, and five developed malaria later than the unvaccinated controls. This sterile protection and delayed patency correlated with the frequency of monofunctional IFN-y-producing CD8+ T cells and not with antibodies, which was the first report of a CD8+ T cell correlate of vaccine--induced protection in humans.[1] This work paves the way for CD8+ T-cell-based vaccines for many other infectious and non-infectious diseases.
REFERENCES:
[1] [a],[b],[c],[d],[e],[f] Ewer KJ, O'Hara GA, Duncan CJ, Collins KA, Sheehy SH, Reyes-Sandoval A, Goodman AL, Edwards NJ, Elias SC, Halstead FD, Longley RJ, Rowland R, Poulton ID, Draper SJ, Blagborough AM, Berrie E, Moyle S, Williams N, Siani L, Folgori A, Colloca S, Sinden RE, Lawrie AM, Cortese R, Gilbert SC, Nicosia A, Hill AV. Protective CD8+ T-cell immunity to human malaria induced by chimpanzee adenovirus-MVA immunisation. Nat Commun. 4, 2836 (2013).
[2] [a],[b] Ogwang C, Kimani D, Edwards NJ, Roberts R, Mwacharo J, Bowyer G, Bliss C, Hodgson SH, Njuguna P, Viebig NK, Nicosia A, Gitau E, Douglas S, Illingworth J, Marsh K, Lawrie A, Imoukhuede EB, Ewer K, Urban BC, S Hill AV, Bejon P; MVVC group. Prime-boost vaccination with chimpanzee adenovirus and modified vaccinia Ankara encoding TRAP provides partial protection against Plasmodium falciparum infection in Kenyan adults. Sci Transl Med. 7, 286re5 (2015).
[3] Bejon P, Andrews L, Andersen RF, Dunachie S, Webster D, Walther M, Gilbert SC, Peto T, Hill AV. Calculation of liver-to-blood inocula, parasite growth rates, and preerythrocytic vaccine efficacy, from serial quantitative polymerase chain reaction studies of volunteers challenged with malaria sporozoites. J Infect Dis. 191, 619 (2005).
[4] [a],[b]McConkey SJ, Reece WH, Moorthy VS, Webster D, Dunachie S, Butcher G, Vuola JM, Blanchard TJ, Gothard P, Watkins K, Hannan CM, Everaere S, Brown K, Kester KE, Cummings J, Williams J, Heppner DG, Pathan A, Flanagan K, Arulanantham N, Roberts MT, Roy M, Smith GL, Schneider J, Peto T, Sinden RE, Gilbert SC, Hill AV. Enhanced T-cell immunogenicity of plasmid DNA vaccines boosted by recombinant modified vaccinia virus Ankara in humans. Nat Med. 9, 729 (2003).
[5] Moorthy VS, Imoukhuede EB, Milligan P, Bojang K, Keating S, Kaye P, Pinder M, Gilbert SC, Walraven G, Greenwood BM, Hill AS. A randomised, double-blind, controlled vaccine efficacy trial of DNA/MVA ME-TRAP against malaria infection in Gambian adults. PLoS Med. 1, e33 (2004).
[6] Draper SJ, Moore AC, Goodman AL, Long CA, Holder AA, Gilbert SC, Hill F, Hill AV. Effective induction of high-titer antibodies by viral vector vaccines. Nat Med. 14, 819 (2008).
[7] Tiono A, Ouedraogo IN, Yaro JB, Ewer KJ, Bougouma EC, Soulama I, Roberts R, Diarra A, Ouedrago A, Lawrie A, Coulibaly S, Rampling T, Bliss C, Barry A, Petersen I, Bowyer G, Anagnostou N, Viebig N, Imoukhuede EB, Bejon P, Hill AVS, Sirima S. Efficacy, safety and immunogenicity of heterologous prime-boost immunization with the candidate malaria vaccines ChAd63 ME-TRAP and MVA ME-TRAP in 5-17 month old Burkinabe infants and children. Am J Trop Med Hyg. 91 (Suppl 5, Meeting Program), 485 (2014).
[8] RTS,S Clinical Trials Partnership. Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet S0140-6736, 60721 (2015).
[9] Alcock R, Cottingham MG, Rollier CS, Furze J, De Costa SD, Hanlon M, Spencer AJ, Honeycutt JD, Wyllie DH, Gilbert SC, Bregu M, Hill AV. Long-term thermostabilization of live poxviral and adenoviral vaccine vectors at supraphysiological temperatures in carbohydrate glass. Sci Transl Med. 2, 19ra12 (2010).
[10] Colloca S, Barnes E, Folgori A, Ammendola V, Capone S, Cirillo A, Siani L, Naddeo M, Grazioli F, Esposito ML, Ambrosio M, Sparacino A, Bartiromo M, Meola A, Smith K, Kurioka A, O'Hara GA, Ewer KJ, Anagnostou N, Bliss C, Hill AV, Traboni C, Klenerman P, Cortese R, Nicosia A. Vaccine vectors derived from a large collection of simian adenoviruses induce potent cellular immunity across multiple species. Sci Transl Med. 4, 115ra2 (2012).
[11] Reyes-Sandoval A, Berthoud T, Alder N, Siani L, Gilbert SC, Nicosia A, Colloca S, Cortese R, Hill AV. Prime-boost immunization with adenoviral and modified vaccinia virus Ankara vectors enhances the durability and polyfunctionality of protective malaria CD8+ T-cell responses. Infect Immun. 78, 145 (2010).
[12] Capone S, Reyes-Sandoval A, Naddeo M, Siani L, Ammendola V, Rollier CS, Nicosia A, Colloca S, Cortese R, Folgori A, Hill AV. Immune responses against a liver-stage malaria antigen induced by simian adenoviral vector AdCh63 and MVA prime-boost immunisation in non-human primates. Vaccine 29, 256 (2010).
[13] O'Hara GA, Duncan CJ, Ewer KJ, Collins KA, Elias SC, Halstead FD, Goodman AL, Edwards NJ, Reyes-Sandoval A, Bird P, Rowland R, Sheehy SH, Poulton ID, Hutchings C, Todryk S, Andrews L, Folgori A, Berrie E, Moyle S, Nicosia A, Colloca S, Cortese R, Siani L, Lawrie AM, Gilbert SC, Hill AV. Clinical assessment of recombinant simian adenovirus ChAd63: a potent new vaccine vector. J Infect Dis. 205, 772 (2012).
[14] Ogwang C, Afolabi M, Kimani D, Jagne YJ, Sheehy SH, Bliss CM, Duncan CJ, Collins KA, Garcia Knight MA, Kimani E, Anagnostou NA, Berrie E, Moyle S, Gilbert SC, Spencer AJ, Soipei P, Mueller J, Okebe J, Colloca S, Cortese R, Viebig NK, Roberts R, Gantlett K, Lawrie AM, Nicosia A, Imoukhuede EB, Bejon P, Urban BC, Flanagan KL, Ewer KJ, Chilengi R, Hill AV, Bojang K. Safety and immunogenicity of heterologous prime-boost immunisation with Plasmodium falciparum malaria candidate vaccines, ChAd63 ME-TRAP and MVA ME-TRAP, in healthy Gambian and Kenyan adults. PLoS ONE 8, e57726 (2013).



